The Ultimate Guide to Pelvic Floor Physical Therapy: The Neurological Edition
When you are diagnosed with a neurological condition, physical and occupational therapy become an important part of your rehabilitative journey. While you’ve likely worked on your strength, mobility, and fine motor skills to aid in improving how you walk, your posture, and other activities of daily living, chances are no one has discussed another important aspect of your care - your pelvic health. As a Doctor of Physical Therapy and neuro-pelvic health specialist, I am here to provide you with the ultimate guide to pelvic floor physical therapy for those with neurological conditions.
In this blog, we’re going to break down everything you need to know about pelvic floor PT and how it can help you in your recovery whether your goals are to maximize your quality of life or regain function during your rehab process.
Below you will find the answers to the following questions:
Why does the pelvic floor need therapy if I have a neurological condition or diagnosis?
What neurological-based pelvic health diagnoses can be treated in pelvic PT?
What does neurogenic bladder and bowel mean?
How can sexual health and function be impacted by a neurological diagnosis?
What other implications does a neurological diagnosis have on my pelvic floor health?
What neurologic diagnoses are treated in pelvic floor therapy?
What goes into becoming a neuro-pelvic health specialist?
How do I find a pelvic floor therapist who specializes in neurological conditions?
What should I expect at the pelvic floor evaluation?
What about at the follow-up visits?
What are the results that someone can expect from pelvic PT?
I noticed a lot of pelvic therapists are out of network, why is that?
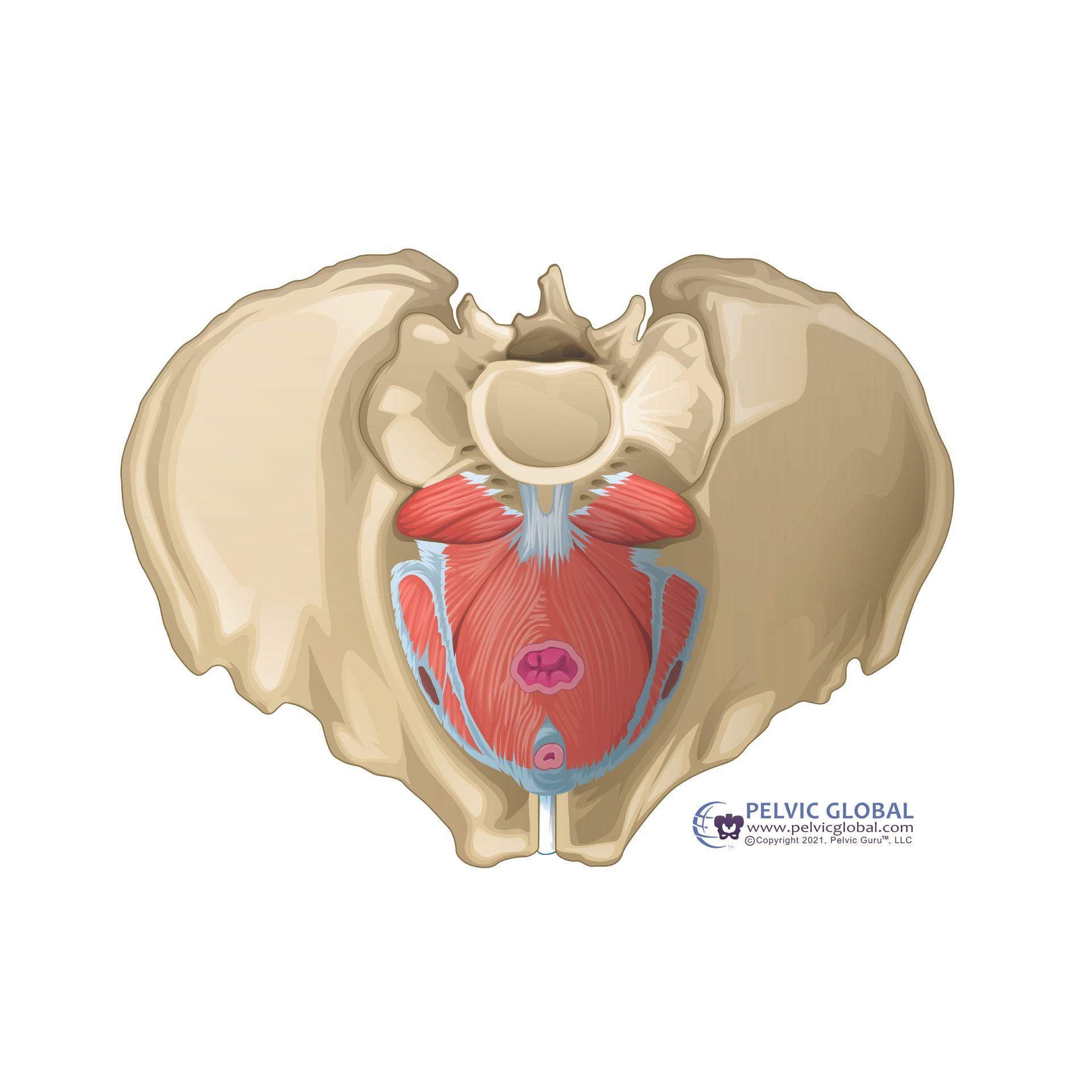
The pelvic floor consists of three layers of muscles that attach to the bottom of the pelvis from the pubic bone (in the front) to the tailbone (in the back). There are also muscles that wrap around the urethra, the genitals, and the anus, some that connect into ligamentous structures to provide support, and one on each side that also serves as a hip rotator. These structures can be observed in the drawings below.
Image used with permission from Pelvic Guru®, LLC as a member of the Global Pelvic Health Alliance Membership (GPHAM)
The pelvic floor muscles serve a variety of functions including:
- Support of the abdominal contents, reproductive organs, bladder & rectum
- Sphincter control around the urethra to keep urine in, when needed, and anus to keep gas and stool in, when needed
- Urge suppression through the pelvic floor and bladder connection to decrease the need to go to the bathroom more frequently (did you know going to the bathroom every 3-4 hours is the norm? Unless you are pregnant or over 65, if you go more frequently you should see a pelvic therapist!)
- Sexual appreciation through strong and well coordinated muscles as this is necessary for achieving orgasm (muscles that are too tight or won’t relax may impact your ability to orgasm)
- Stabilization along with the abdominal muscles and in coordination with the diaphragm during things like coughing, laughing, sneezing, running, jumping, lifting heavy objects, and just moving our body around day to day
The pelvic floor muscles, like any skeletal muscle in the body, serve these functions through a series of complex pathways and reflexes in our nervous system. Keep reading to learn more!
Why does the pelvic floor need therapy if I have a neurological condition or diagnosis?
Great question! To answer this question, let’s start with a brief review of the anatomy and role of our nervous system. The nervous system consists of the brain, spinal cord, and peripheral nerves (nerves that run through your body, all the way to your fingers and toes). Your nervous system’s main function is to send messages from various parts of your body to your brain and from your brain back out to your body, to tell your body what to do. These messages regulate your thoughts, memory, learning, and movements, including balance, posture, strength, and coordination.
With a neurological condition, the sensory and motor communication between the brain, spinal cord, peripheral nerves, and subsequently, the muscles throughout the body can be impacted. Just like you may have previously experienced, or continue to experience, strength, sensation, and coordination changes to the arms, legs, trunk, and face, the pelvic floor muscles can also be weak, tight, stiff, or discoordinated due to an injury to the nervous system.
This may lead to things like leaking urine or feces, frequent or urgent need to use the bathroom, urinary retention or urine stream changes, sexual dysfunction, pain, or difficulty with pelvic exams or using menstrual products. These symptoms may be new following the onset of your injury or diagnosis and may change or intensify with the course of your condition depending on the chronicity, episodic, or progressive nature of your neurologic diagnosis.
With that said, pelvic floor therapy is here to help support and maximize your pelvic floor muscle function no matter where you are in your journey! Pelvic floor therapy may include working on the strength, flexibility, coordination, and awareness of the pelvic floor muscles to improve, support, and best maintain function of your bowel, bladder, and sexual health.
What neurological-based pelvic health diagnoses can be treated in pelvic PT?
As noted above, an injury or insult to the nervous system - whether to the brain, spinal cord, and/or peripheral nerves - can play a significant role in bowel or bladder health, and sexual function.
At Pelvic Pride we treat the following pelvic health diagnoses specific to a neurologic condition:
Neurogenic Bowel
- Fecal incontinence (leaking stool)
- Fecal urgency (a strong need to go)
- Constipation
Neurogenic Bladder
- Urinary Incontinence (leaking urine)
- Urinary urgency or frequency (a strong or frequent need to go)
- Urinary retention (difficulty emptying the bladder)
- Having an ‘elevated or a high PVR’ (PVR - post-void residual) can indicate urinary retention and/or difficulty emptying your bladder which is a common symptom reported by individuals affected by a neurologic condition.
- Difficulty starting urine stream or weak urinary stream
Neurogenic Erectile Dysfunction and other Sexual Health Changes
- Difficulty achieving orgasm
- Incomplete orgasm
- Difficulty achieving or maintaining erection
- Premature ejaculation
- Pain with sex
Other pelvic health diagnoses may also impact someone with a neurological condition or may have been present prior to a condition’s onset, including pelvic pain, pelvic organ prolapse, and any difficulties associated with pregnancy and postpartum, including diastasis rectus abdominis.
For a comprehensive list of diagnoses we treat please check out the Conditions We Treat.
What does neurogenic bladder and bowel mean?
Neurogenic bowel and bladder is an umbrella term used to describe any urinary or bowel condition in individuals who lack control due to a brain, spinal cord, and/or nerve problem/injury.
The bowel and bladder functions through a series of neural pathways and reflexes under a combination of voluntary and involuntary control. The gastrointestinal tract is also regulated by its own nervous system called the enteric nervous system. Further, our bowel and bladder communicate with the brain via our peripheral nerves and spinal cord, as well as with our pelvic floor muscles to coordinate bowel and bladder filling, storage, and emptying. If there is an injury or dysfunction anywhere along these pathways, this can impact the body’s ability to store or empty urine or feces.
Those that suffer with neurogenic bladder or bowel may report urinary or fecal urgency, frequency, constipation, leakage associated with urgency or stress on the system (cough, laugh, sneeze, or standing up), weak urinary stream, small urine volumes, urinary retention, urinary hesitancy, and frequent nighttime urination.
So how can pelvic therapy help with neurogenic bowel and bladder?
Your pelvic health therapist will offer strategies for bowel and bladder routine support, toileting setup and positioning strategies, fall risk assessment, caregiver education and training. During your therapy sessions you will also work on breathing exercises, lumbo-pelvic strengthening, and pelvic floor muscle coordination training. Our goal is to help you become as independent as possible and gain or maintain control over your bodily functions.

How can sexual health and function be impacted by a neurological diagnosis?
Sexual function requires appropriate interaction between multiple pathways, including our neurological, hormonal, vascular, and psychological systems. A neurological condition can directly impact the brain centers associated with sexual libido/desire, and the spinal cord and nerves needed to communicate signals regarding sensation, motor, and vascular changes for genital engorgement, arousal, and lubrication. Our pelvic floor muscles also play an important role in sexual health, including blood flow, tissue engorgement and erection, lubrication, and orgasm. A person with a neurologic condition may report impaired arousal or lubrication, diminished or absent orgasm, sensation loss or changes, erectile dysfunction, or premature ejaculation.
Your pelvic health therapist will offer:
- techniques for sexual routine support, setup and positioning strategies
- partner(s) education and training
- energy conservation techniques
- adaptive/assistive equipment and tool recommendations
- stretches
- breathing exercises
- strengthening
- soft tissue mobilization
- hands-on external or internal pelvic floor work
In addition, your pelvic health therapist may discuss other important components to sexual libido, desire, and arousal, including erogenous zones - certain places on the body that have a heightened sensitivity and can elicit a sexual response when stimulated (think lips, neck, nipples, and inner thighs to name a few). Finding strategies to elicit areas of the body outside the genitals and pelvic floor musculature that may have intact or improved sensation can be beneficial to maximizing your sexual health goals.
What other implications does a neurological diagnosis have on my pelvic floor health?
Bowel and bladder and pelvic floor muscle health and function can also be impacted due to medication side effects, impaired mobility including difficulties with getting to the toilet in time or managing doffing clothing, cognitive changes, dietary changes, spasticity (or stiff muscles), and fatigue.
Like bowel and bladder health, sexual function can additionally be impacted by mobility difficulties, muscle weakness or stiffness impacting postural stability and comfort in certain positions, bowel and bladder control issues, fatigue, tremors, cognitive changes, as well as concurrent conditions, including hypertension, anxiety, and depression.
What neurologic diagnoses are treated in pelvic floor therapy?
Neurogenic bowel, bladder, and sexual dysfunction symptoms can occur due to a number of neurological conditions, including but not limited to:
- Traumatic and nontraumatic brain injury (TBI)
- Stroke (CVA)
- Multiple sclerosis (MS)
- Parkinson’s disease (PD)
- Spinal cord injury (SCI)
- Cerebral palsy (CP)
- Spina bifida
Keep reading to learn more about how the pelvic floor muscles may be impacted specific to each diagnosis!
In addition to listed diagnoses above, we at Pelvic Pride work with individuals navigating other neurologic conditions, including post-concussion syndrome, tethered cord, transverse myelitis, and Guillain-Barré syndrome (GBS), to name a few. Please feel free to give us a call for a free phone screening to learn if pelvic therapy may be a right fit for you!
Traumatic and Non-Traumatic Brain Injury
Following a TBI or non-traumatic brain injury such as a stroke, individuals commonly report changes to the urinary system (retention, leakage, and a weak urine stream) and gut (constipation, fecal urgency). Catheterization is common following a TBI or stroke to assist with emptying of bladder and may or may not continue to be part of a person's daily bladder routine depending on severity of injury and course of recovery post-insult. Individuals can also experience changes in the strength and sensation of the genital tissue and pelvic floor muscles thus impacting sexual arousal, erection, and orgasm. Further, TBI’s are commonly associated with additional bodily injury, including spinal, pelvic, or extremity fractures, organ damage, and potential scar tissue from surgical procedures which commonly affect bowel, bladder, and pelvic function and healing. Pelvic health PT can assist with finding techniques to improve independence and safety with toileting routines, offer caregiver education and support, and strategies to support return to sexual health.
Multiple Sclerosis
Those affected by Multiple Sclerosis (MS) may report changes to the urinary system (urinary urgency, frequency, leakage, retention, and straining to empty) and gut (constipation, fecal leakage). Catheterization is common to assist with emptying of the bladder when urinary retention or difficulty voiding is reported. Sexual function may also be impacted (decreased libido, erectile dysfunction, incomplete or absent orgasm, lack of lubrication) and can be affected by secondary factors including fatigue, muscle spasticity and weakness, hormone changes, as well as mental and emotional changes including depression.
In conjunction with any disease-modifying therapy treatments a person with MS may be navigating with their medical team, a pelvic health therapist can be another helpful member of your team! Pelvic therapists can assist with
- finding techniques to improve symptoms of constipation
- independence and safety with mobility to/from bathroom to decrease the risk of falls
- energy conservation strategies to address fatigue
- pelvic floor muscle training which may assist with urinary leakage
- strategies to support sexual health such as positioning education to improve comfort
- toy or equipment recommendations as vaginal vibration may improve orgasm and sexual arousal
Pelvic therapy will also discuss pregnancy, birthing, and education on postpartum preparation, as changes in relapses and symptoms can occur during pregnancy or postpartum. Pelvic floor therapists can also be on your medical team to support overall symptoms depending on disease progression.
Parkinson’s Disease
Individuals with Parkinson’s Disease may commonly report changes to the urinary system (urinary urgency, frequency, and leakage as bladder inhibition is reduced due to decreased dopamine levels) and gut (constipation being the most common symptom in both early and late stages of the disease). Individuals may also notice sexual function may be impacted (decreased libido, erectile dysfunction). Pelvic health PT can assist with finding techniques to:
- improve symptoms of constipation
- establish voiding schedules
- urge suppression to ‘buy the bladder time’ for independence and safety with mobility to/from bathroom
- equipment recommendations
- offer caregiver education/support
- provide strategies to support sexual health.
Spinal Cord Injury
Following a spinal cord injury, whether traumatic or non-traumatic in nature, individuals commonly report changes to the urinary system (retention, leakage, recurrent UTIs, and decreased bladder urge sensation) and gut (constipation, fecal leakage), as well with sexual function (changes in sensation to genital region and pelvic floor muscles, difficulty with arousal, incomplete or absent orgasm, erectile dysfunction). A patients’ symptoms will vary based on the level and severity of their injury. Catheterization is common to assist with emptying of the bladder for long-term management following a spinal cord injury.
Pelvic health PT can assist with finding techniques to:
- improve bladder routines including discussion of equipment or orthosis support
- improve constipation and establish/support your bowel program
- improve independence and safety with mobility to/from bathroom
- offer caregiver education and support
- provide strategies to support sexual health, including
- positions for improved stability and comfort
- toy or sexual enhancement device recommendations
- discussion of maximizing intact sensation areas, such as erogenous zones, for arousal and orgasm
Cerebral Palsy & Spina Bifida
Individuals with cerebral palsy (CP) commonly report neurogenic bladder changes (urinary retention and leakage most commonly due to spastic bladder), neurogenic bowel changes (constipation, fecal leakage), decreased mobility, communication difficulties, and side effects of certain mediations. Pelvic health PT can assist with finding techniques for:
- improved toileting positioning due to lower extremity stiffness or spasticity
- bowel routine support recommendations
- timed voiding
- offer caregiver education and support
- review movement and positioning for improved sexual function
Individuals with Spina Bifida may commonly report changes to the urinary system (urinary retention, urgency, frequency, and leakage) and gut (constipation, fecal leakage). Catheterization may be utilized to assist with emptying of the bladder. Sexual function can be impacted by changes in genital and pelvic floor muscle sensation depending on the level of injury, symptoms such as urinary leakage during sexual activity, and daily routines and needs, including catheterization and bowel programs. Pelvic health therapy can assist with finding techniques to:
- improve symptoms of constipation
- fluid recommendations
- independence and safety with mobility to/from bathroom
- equipment recommendations
- offer caregiver education and support
- review catheterization and bowel routine schedules for improved sexual function
What goes into becoming a neuro-pelvic health specialist?
Pelvic health physical and occupational therapists have their initial base coursework and training from their respective physical and occupational therapy graduate programs. From there, therapists complete additional coursework and training in order to specialize in pelvic health therapy, which includes external and internal pelvic floor muscle assessment and treatment. Pelvic health therapists can then take additional coursework in the education, evaluation, and treatment of individuals navigating pelvic health difficulties associated with a neurological condition.
In addition to traditional coursework, a physical therapist’s background and experience can play a role. As an example, prior to joining the Pelvic Pride team, I specialized in working with individuals with neurological diagnoses, including TBI and Stroke, in a hospital setting to improve function and mobility prior to transitioning to the pelvic health speciality, and continues to apply this knowledge in my pelvic health practice.
How do I find a pelvic floor therapist who specializes in neurological conditions?
If you’re looking for a pelvic floor therapist in your area (and you are not local to Baltimore, MD where Pelvic Pride is located), then we suggest checking out the following directories to find a pelvic therapist:
If you are located near Baltimore Maryland, we’d love to help you here at
Pelvic Pride.
Keep in mind, not all pelvic health PT/OT’s work with the neurological population in pelvic health. If you are looking specifically for a provider who can help with a neurological condition, I advise that you call the specific practice or facility to inquire further, prior to booking.
Here are a few questions that may be helpful to ask when looking for a neuro-pelvic provider:
- Does your facility treat conditions like neurogenic bowel, bladder, and/or erectile dysfunction as a result of a neurological condition?
- Does your facility have pelvic health therapists trained in working with a person with a neurologic condition?
- What is the accessibility of your facility or clinic? This may include discussing wheelchair accessibility, parking, bathroom accessibility, and equipment accessibility.
What should I expect at the pelvic floor evaluation?
While each clinic is different, at Pelvic Pride we allot 75 minutes for your evaluation. During this time we want you to share your story and explain your symptoms, tell us about any providers you have seen and share any testing that has been completed already. (Be sure to fill out any intake paperwork ahead of time and put down as much information as you feel comfortable sharing as this will help make sure you don’t forget anything.)
As you go, your provider should ask questions to gather more information and start to better understand your symptoms and their possible causes. Once this portion of the evaluation is done, you will move into the hands-on assessment. This may include assessing the range of motion, flexibility, strength and/or soft tissue restrictions of various areas from head to toe (depending on what brings you to therapy). This may also include a hands-on pelvic internal examination.
Doing an internal examination will give your provider more information about your pelvic floor muscles including if they are tight, weak, coordinated, or struggle to relax. It is important to note that while an internal assessment is helpful, it is
never required
and your
enthusiastic consent should be gained by your provider prior to performing an internal exam. If you wish to defer the internal assessment, there are plenty of other options that your provider should offer you instead.
Once the assessments have been completed, your provider should review their findings and guide you in some treatment options which may include things you can do at home before your next appointment.

What about at the follow-up visits?
Again, we feel like time is so important, therefore we offer full 60-minute follow up appointments, one-on-one with your provider. At Pelvic Pride we don’t change providers unless it is requested or we discuss how that may be helpful.
Keep in mind that it may take a few visits to complete all of the evaluative assessments needed, therefore your first few sessions may be a mix of assessment and treatment. Once your provider has finished their evaluation testing, your sessions should focus on education regarding the root cause of your symptoms and treatment to best support your symptoms with a goal to maximize any intact sensation or motor function. This may include bowel and bladder routine support, toileting position strategies, fall risk assessment, caregiver education and training, as well as stretches, breathing exercises, strengthening, soft tissue mobilization, or hands-on external or internal pelvic floor work.
If you want to learn more check out our blog post on
The 3 Treatment Methods of Pelvic Therapy.
What are the results that someone can expect from pelvic PT?
Great question! Although a pelvic-neuro pelvic health therapist cannot revert, alter, or prevent any pathological nervous system changes due to a progressive or non-progressive neurological condition, our goal is to find treatment techniques and strategies that best support your symptoms and help you improve your quality of life.
While each patient presents differently, things we typically may see with our patients who have neurological diagnoses include:
- Improved daily bowel habits and routine to address constipation
- Improved urinary or bowel leakage that may occur with daily tasks including functional mobility like transfers or walking, trying to get to the bathroom on time, or during sexual activity
- Improved urinary frequency, urgency, and/or retention
- Improved sexual function including improved orgasm, erectile function, and positional support
- Decreased pelvic, low back, or hip pain and tightness and conservative support techniques for spasticity management
- Improved mobility and decreased pain or stiffness associated with potential scar tissue as a result of a traumatic event
- Improved awareness and coordination of the lumbo-pelvic musculature, including pelvic floor, abdominals, spinal, and hip muscles, dependent on intact innervation of these muscles
- Improved overall knowledge of the anatomy and function of the nervous system (brain, spinal cord, and nerves) and connection with the bladder, bowel, and genital structures
It is likely that your pelvic PT will want to communicate with other members of your medical team, including urology, gastrointestinal, neurology, to ‘quarterback’ your care via interdisciplinary collaboration for holistic support and care. Further, your medical team may incorporate additional testing or imaging to learn more about your symptoms (such as urodynamic testing to assess bladder function) and discuss medication management for symptom support, including medications that can address spasticity, discomfort or pain associated with nerves, or anxiety and depression.

Insurance companies do not look at pelvic floor therapy as a different type of therapy than standard physical/occupational therapy. So, if you have coverage for those services then yes, insurance will pay for pelvic floor therapy, BUT…
There are big limitations placed on physical/occupational therapy by the insurance companies in the form of visits limits (your plan will dictate how many sessions they cover), denial for certain diagnoses (they feel PT/OT is ‘experimental’ treatment for certain diagnoses), and the decision to discontinue coverage for PT/OT if they determine it is no longer medically necessary. We also recognize that living with a neurological condition can be a lifelong journey and may be episodic and/or progressive in nature and recognize that patients may require ongoing therapy to help manage their chronic symptoms, which insurance does not like.
I noticed a lot of pelvic therapists are out of network, why is that?
While looking for pelvic floor providers, it will not be uncommon to find that many are considered ‘out-of-network’ meaning they do not have a relationship with insurance companies. This means the patient will pay for their sessions at time-of-service and can submit receipts to insurance for reimbursement. This is the model we offer at Pelvic Pride as we feel it allows the provider to work with the patient and determine the best plan of care for their symptoms, without the limitations we previously discussed from insurance companies. This also prevents the issue of a surprise bill at any point in your care (this typically occurs when the insurance stops paying or the visit limit is reached however the therapy clinic does not realize this until the patient has been seen past those limits, then the cost is put onto the patient). At Pelvic Pride, you will know up front what the cost is each time and you will never get a big bill at the end.
Do you want to dive into this a little deeper? Read our blog for more on
Why Choose A Fee-For-Service Physical Therapist.

How do I know if I need pelvic PT?
Excellent question! Luckily we have a quick screening tool for that. Read through the 10 questions and keep in mind, if you say ‘yes’ to 3 or more questions, it is likely you have pelvic floor dysfunction and would benefit from seeing a pelvic health therapist.
Where to find treatment in Maryland
At Pelvic Pride Physical Therapy & Wellness, we specialize in the treatment of ALL pelvic floor conditions, including neurologic conditions, so you are in the right place! We are conveniently located in the Federal Hill neighborhood in Baltimore MD. Fill out our contact form & our Patient Care Specialist will reach out to you ASAP!
Next on Your Reading List
Love our content? Let's stay connected!
Subscribe to our newsletter for personalized updates when new blog posts are dropped.